Other Liver Disorders
What are autoimmune liver disorders?
An autoimmune disorder is any reaction or attack of a person's immune system against its own organs and tissues. In the liver, the immune system can destroy liver cells and damage bile ducts. Chronic hepatitis can be caused by an autoimmune disorder.
What are metabolic liver disorders?
Two main metabolic disorders affect the liver:
- Hemochromatosis - the absorption of too much iron from food. The excess iron is stored throughout the body, including in the liver and pancreas. This excess iron can damage these organs. Hemochromatosis is a hereditary disease that can lead to liver disease, liver failure, liver cancer, heart disease and diabetes.
Wilson's Disease - the retention of too much copper in the liver. Instead of releasing the copper into the bile, the liver retains the copper. Eventually the damaged liver releases copper into the bloodstream. This hereditary disease can cause damage to the kidneys, brain and eyes, and lead to severe brain damage, liver failure and death.
Biliary Diseases (bile obstruction)
Biliary Atresia (congenital disorder)
Biliary atresia is the congenital absence or closure of the ducts that drain bile from the liver. It is a progressive process that begins very soon after birth. Bile is trapped inside the liver and rapidly causes damage and scarring to the liver cells. Further scarring of the liver tissue may result in cirrhosis.
Diagnosis
- Jaundice after the age of 2 to 3 weeks.
- Yellow eyes and skin, light-colored stools and dark urine.
- The abdomen may be swollen with a firm, enlarged liver.
- Weight loss and irritability develop as the level of jaundice increases.
- Blood tests: increased bilirubin (a chemical marker in the blood for jaundice).
- An ultrasound test may detect an absent or tiny gall bladder.
- HIDA scan - Liver biopsy
- Intraoperative Cholangiography confirmatory test
Treatment Operation
Once the diagnosis is confirmed, the preferred treatment is to perform surgery and remove the blocked biliary ducts outside the liver and attach the small intestine directly to the liver at the spot where bile is found or expected to drain (called Kasai procedure). Early diagnosis of this disease is very important. If surgery is performed before the baby is 2 months old, success is much more likely. About 30% are benefited permanently, 50% only partially, whereas 20% are not benefited by operation. For those who do not respond to corrective surgery, the liver damage continues and cirrhosis develops. Progressive cirrhosis will eventually require liver transplantation.
Liver transplantation plays an important role in the long-term treatment of biliary atresia. Pediatric liver transplantation has evolved into a highly successful therapy and now offers significant hope for all children born with biliary atresia.
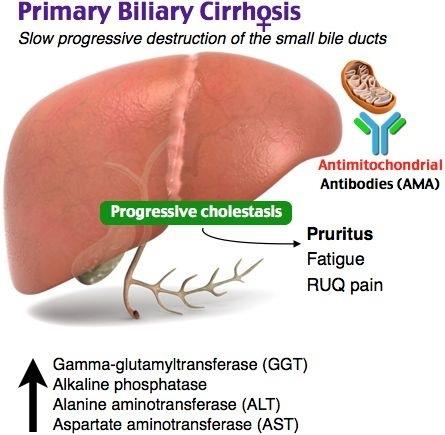
Primary Biliary Cirrhosis (PBC)
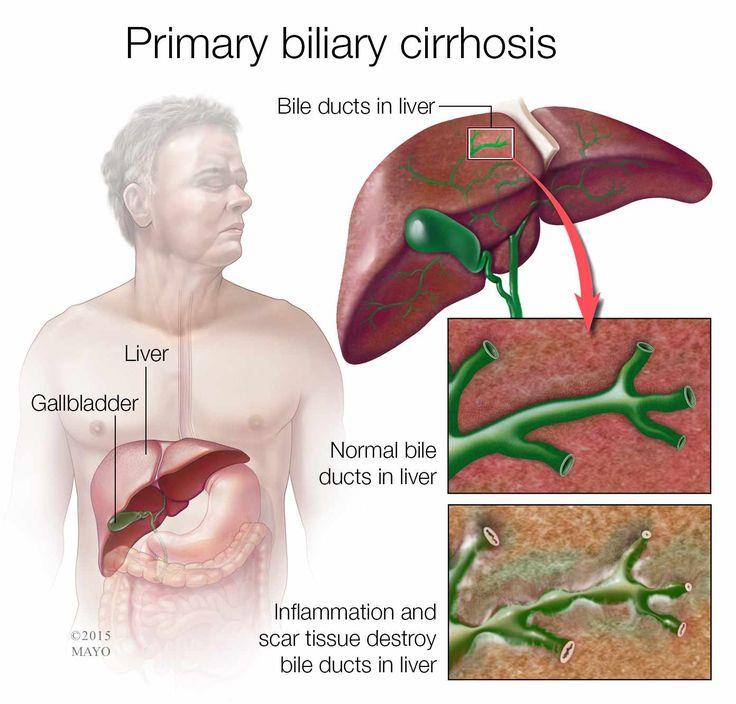
Primary biliary cirrhosis is a liver disease that slowly destroys the bile ducts in the liver. Bile, a substance that helps digest fat, leaves the liver through these ducts. When the ducts are damaged, bile builds up in the liver and damages liver tissue. Over time, the disease can cause cirrhosis and may make the liver stop working.
The cause of primary biliary cirrhosis is unknown. The disease affects women more often than men, and usually occurs between the ages of 30 and 60 years. Some research suggests that the disease might be caused by a problem within the immune system.
The most common symptoms of primary biliary cirrhosis are itchy skin and fatigue. Other symptoms include jaundice (yellowing of the eyes and skin), cholesterol deposits on the skin, fluid retention, and dry eyes or mouth. Some people with primary biliary cirrhosis also have osteoporosis, arthritis, and thyroid problems.
Primary biliary cirrhosis is diagnosed through laboratory tests, x rays, and in some cases, a liver biopsy (a simple operation to remove a small piece of liver tissue). Treatment may include taking vitamin and calcium supplements, hormone therapy, and medicines to relieve symptoms. Ursodiol is beneficial for patients with primary biliary cirrhosis although it does not cure the disease. A liver transplant may be necessary if the liver is severely damaged.
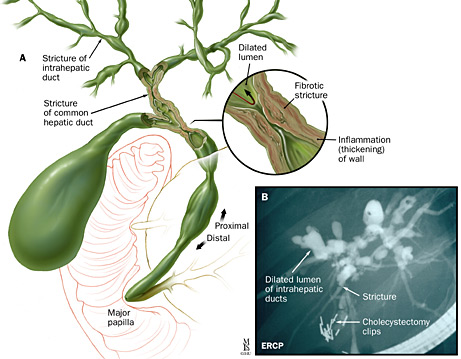
Primary Sclerosing Cholangitis (PSC)
In primary sclerosing cholangitis (PSC), the bile ducts inside and outside the liver become inflamed and scarred. As the scarring increases, the ducts become blocked. The ducts are important because they carry bile out of the liver. Bile is a liquid that helps break down fat in food. If the ducts are blocked, bile builds up in the liver and damages liver cells. Eventually, PSC can cause liver failure.
Researchers do not know what causes PSC. Among the theories under investigation are the possible role of bacteria, viruses, and immune system problems. PSC appears to be associated with ulcerative colitis, a type of inflammatory bowel disease.
The disease usually begins between ages 30 and 60, but the disease can also arise during childhood. PSC is more common in men than women. PSC progresses slowly, so a person can have the disease for years before symptoms develop. The main symptoms are itching, fatigue, and jaundice, which causes yellowing of the eyes or skin. An infection in the bile ducts can cause chills and fever.
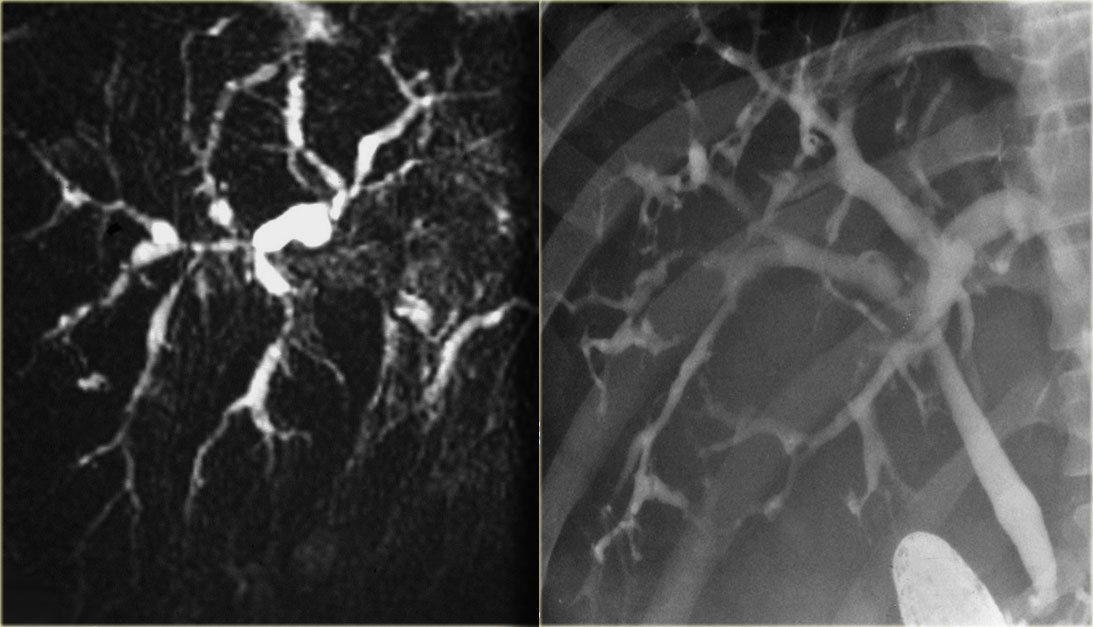
PSC is diagnosed through cholangiography, which involves injecting dye into the bile ducts and taking an x ray. Cholangiography can be performed as an endoscopic procedure (endoscopic retrograde cholangiopancreatography, ERCP), through radiology or surgery, or with magnetic resonance imaging (MRI) scans. Treatment includes medication to relieve itching, antibiotics to treat infections, and vitamin supplements, as people with PSC are often deficient in vitamins A, D, and K. In some cases, surgery to open major blockages in the common bile duct is also necessary. Liver transplantation may be an option if the liver begins to fail.